Philosophical study of life, death, and nature
Home > Books > Brain Dead Person (general info.) > This page
Philosophical study of life, death, and natureHome > Books > Brain Dead Person (general info.) > This page
|
 |
|
Brain-Dead Person Masahiro Morioka > General information of this book
Chapter 1
What Doctors Cannot See Many theories about brain death have been written from doctor's perspectives.It stands to reason that brain surgeons, who know the most about the medical state of brain death, and conduct research about the brain, should write books about brain death. But this does not mean that brain surgeons understand the essence of brain death.They only understand the medical aspect of brain death.They know nothing about the thoughts or feelings a family might have as they stand before a brain dead relative, and nothing about how defining 'brain death' as 'human death' could affect culture and society. The real issue of brain death does not concern the medical aspect, but how we should treat brain dead people in society. [3/4] What we, as the 'general public', want to know, is not the medicine of brain death, but how we should interact with brain dead people. Let me try to explain this point; there is a book titled Theories of Brain Death: the Meaning of Living and Dying (Soshisha, Dec., 1986) written by a brain surgeon, Dr. Hiroshi Mizutani.I recommend this book, as it is written from a broad perspective. The first chapter of this book begins as follows:
The book goes on to describe the functions of the limbic system, the brain stem, and the spinal cord. A large cross section of the brain is shown two pages after that. When writing this book, the author begins with the brain functions and the cross section of the brain. So it could be said that Dr. Mizutani's theory on brain death is written from a doctor's perspective. Let me cite another example. The book Brain Death (Nihon Kirisutokyo Shuppankyoku, April, 1988) consists of a series of dialogues between a doctor, Tadao Tsubaki, and a theologian, Masakatsu Seki. This book also begins with the heading “What is the State of Brain Death?” and describes blood pressure and a respirator. The authors explain the functions of the cerebrum and the brain stem, then present the same cross section as in Dr. Mizutani’s book. It goes without saying that minimal medical knowledge of brain death is necessary to discuss it. Some critics, such as Takashi Tachibana, say that we should be careful not to go into further discussion before the medical questions are resolved. [4/5]This is one way of thinking, I admit. But what I think is this: Why are there so many people who, when they talk about brain death, start by talking about a cross section of the brain? Perhaps, they think that if we understand perfectly the cross section and how the brain functions, we will understand brain death in its entirety.But all we understand when we understand a cross section and the how the brain functions is the medical aspect. Is brain death just brain death from a doctor's perspective?I don't think so.The real essence of brain death is just what the doctors can't see.Most theories about brain death so far share one common way of looking at it: "If you understand the brain, then you understand brain death." As long as you hold this 'world view' of brain death you will not be able to see its true essence. The meaning of brain death to a family The people who encounter brain death in hospitals can be divided into three kinds.The doctors who specialise in the brain, the nurses who provide care for the patients, and the families who watch over the patients from outside the ICU.Among these, it is the doctors who are concentrating fully on what is happening inside the patient's brain.This is because if they don't understand exactly which part of the brain has been damaged and what state it is in, they cannot provide the appropriate medical treatment. [5/6]This means that the doctors face the 'the inside of the patient's brain'. Nurses are in a slightly different position.The nurses are concentrating on the body of a comatose patient.They are concerned with monitoring the body's condition and checking the status of various kinds of medical equipment surrounding the patient.So it could be said that the nurses are first and foremost facing 'the patient's body'. Similarly, the family are in a different position from the nurses.To a nurse, the patient in front of them is a stranger who they are seeing for the first time, whereas to the family the patient is an irreplaceable blood relative with whom they have spent much of their life. The family are allowed to come into the ICU for a few minutes two or three times a day, where they come face to face with the patient for the first time.At this point the family are facing 'the person known as a patient', who they share a life and past with. Imagine a patient falls into a state of brain death in spite of strenuous medical efforts. The family are brought into the ICU and the doctor pronounces the patient brain dead.As they listen to the doctor, the family watch their relative lying on the bed.At this point the family are not facing the inside of the patient's brain, nor their body.What they are facing is a person, who has entered a state known as brain death. The average person such as you or I only encounter brain death when a relative of ours becomes brain dead.At that time we are not facing the inside of a dead brain, but a person, a close relative who has become brain dead, or in other words, a brain dead person. Therefore, the real issue you and I are faced with is not 'here is a dead brain',but 'this is a brain dead person'. [6/7] So theories about brain death meant for the general public should not begin with an explanation of a brain, but should take 'the brain dead person' as the starting point for their discussion. Imagine you or I encounter a brain dead parent, child, sibling, grandparent, or friend for the first time in the ICU of a hospital.This is an encounter between two people.This is an encounter between two people, one of which has a working heart and brain, and the other with a non-functioning brain, but a heart that still works. This scene is described vividly in a famous passage by Michi Nakashima.Although it is rather long I would like to quote it here:
Critics might say that this kind of description is sentimentalism and has no place in scientific discussion, or that how the family feels has nothing to do with the hard fact that the patient is brain dead. I think such critics are only seeing half the issue.What families are encountering in the ICU, and what they really see as important, is not a set of hard medical facts about the inside of the brain, nor scientific discussion about the functions of the brain. What the family encounter in the ICU is a 'brain dead person', fixed in a bed and apparently in a deep sleep, with whom they have spent their lives until now, and to whom they say goodbye when the respirator is taken away.Therefore the true nature of this encounter between people is not in scientific data, but in feelings, the realisation of death, the denial of death, and the acceptance of death. A 'person' whose brain has stopped functioning In this way, the family have the most dramatic encounter with the brain dead person.However if you think about it more closely, the nurses caring for the patient's body, as well as the doctors trying to revive the patient's brain also come face to face with the brain dead person.But it seems that they are concentrating too closely on a particular part of the patient to be able to see them as a person. [8/9] We can put it as follows: brain death has always been thought of as the contents of a patient's brain when it ceases to function.However as has already been stated, this nothing more than brain death from a doctor's perspective.Brain death from a doctor's perspective is only one aspect of the broader concept of brain death. Let's try looking at this in a different way.There is a person whose brain has ceased to function in an ICU.Around them are persons called doctors, persons called nurses, persons who are their family, and all kinds of persons related to the hospital, local residents and so on.All of these persons have various relationships to each other based around the person whose brain has ceased to function.For example, the persons who are the family might be pleading with the person known as the doctor to let them see, if only for a moment, the person whose brain has stopped functioning again.Or the person known as the doctor might be worrying about whether or not to take the person whose brain has stopped functioning off the respirator.Or the persons known as nurses might be disinfecting and wiping down the body of the person whose brain has ceased to function in order to prevent infection.Or outside the hospital, persons known as transplant doctors might be calling in to see if they can receive organs from the person whose brain has ceased to function. I would like to define 'brain death' as the sphere, centered around the person whose brain has ceased to function, in which these kinds of person to person relationships exist.'Brain death' is not to be found inside the brain of the person whose brain has ceased to function, but in the sphere of human relationships surrounding that person.What we should be considering is 'brain death as a sphere'. The essence of brain death is to be found in relationships between people.So when a doctor looks at the brain of a person whose brain has ceased to function, they are seeing brain death with a doctor's eyes, which is only one aspect of the whole. [9/10] And of course, if the essence of brain death is to be found in relationships between people, then naturally the question arises of how doctors, nurses, families, transplant staff, residents and people in general should behave in their relationships to one another.This is the ethics of brain death.The essence of brain death is the nature of relationships between people, and this creates the ethical problem of how people should conduct their relationships.And as I will suggest later, the same issue in fact applies to organ transplantation, and the relationships between the people who donate organs, the people who agree to the transplants, the people who receive organs and the people who act as intermediaries between them. The condition of a 'brain dead person' Now I would like to give a basic explanation of the 'brain dead person' around whom all of these person to person relationships occur.First, please imagine three kinds of people:
[10/11] The person 1., whose heart and brain are both functioning is a normal living person like you or I.If we place our hand on our chests we can feel our hearts beating, and our functioning brain allows us to experience all kinds of thoughts and feelings.The person 3. whose heart and brain have both stopped is someone lying cold in a coffin who will never return to life.If you touch them they have no pulse, and they do not react to any kind of stimulus. 1. and 3. are 'persons' that we know well from everyday life.However recently persons like 2. have started to emerge, who, despite having a functioning heart, have a non-functioning brain. According to recent statistics, less than one percent of people near death end up as brain dead people in the ICU of large hospital.In most cases, the state of brain death continues for a few days, then the heart stops and they become a cold dead body. While the state of brain death continues, the brain dead person lies on a bed in an ICU, connected to various life preserving equipment - mainly a respirator - as well as to monitoring equipment, blood transfusion tubes and so on.That is to say, a brain dead person can only exist in the ICU of a large hospital that has the appropriate equipment and expertly trained medical staff.I will explain in detail about what kind of place an ICU is in the next chapter. A brain dead person's heart and lungs function thanks to the respirator, but apparently their brain does not. The condition of a brain dead person is as follows.First they are in a deep sleep known as deep coma, where they do not react even to pain stimulus.For example, even if you were to prick their face with a pin, they would not respond with a grimace. Because they cannot breathe by themselves, they must be assisted by a respirator.If they were taken off the respirator then their breathing would instantly stop and their heart would stop beating.They have lost their brain stem reflex, and so they do not close their eyes if you poke them with a cotton bud, they do not respond to stimulation in the throat and trachea, nor to cold water being poured into the ears. [11/12] Their pupils remains dilated even if bright lights are shone into their eyes, and brain waves are not detected using an encephalograph.This is considered evidence that the cerebrum, which governs the ability to think and have emotions, is not working.There is no possibility of recovery, and in most cases the heart stops beating within a week (there are some exceptions; I will elaborate on them in Chapter 4. For readers interested in the detailed standard for the determination of brain death, please refer to the Nihon Ishikai Zasshi, Vol. 94, No.11, 1985, which features brain death, in which the full text of the so-called Takeuchi report was published. Please consult the Japan Medical Association or a nearby library. It would further your comprehension to read Brain Death by Takashi Tachibana after that.) Thanks to the respirator and medication to boost blood pressure, blood continues to circulate around the body of the brain dead person, and so their body is still warm.As blood is circulating around their body, the brain dead person perspires and accumulates scurf which necessitates regular cleaning.And because water leaves the body as sweat, it needs to be replenished.The brain dead person also excretes, and this needs to be dealt with.Like a bedridden elderly person, the patient may suffer bedsores, so a regular change of position is necessary. Thus, a brain dead person requires all kinds of care. In a hospital, much of this care falls to nurses. Tateo Sugimoto, whose son became brain dead and later died, describes the situation as follows:
A brain dead person is this kind of person.A brain dead person in fact appears as many different people, depending on the viewpoints of the people around them.For example, to the doctors and nurses, a brain dead person is a stranger who is suddenly thrust into the ICU.But to their family, a brain dead person is someone they are close to, who they have shared a life and history with right up until the previous day.By contrast, to a patient in a distant hospital waiting for an organ transplant the brain dead person is nothing more than the abstract image of a person. To my child I could be a good father, to my wife a weary lover, to my colleagues a hardworking employee, and to the barman a happy drunk, and the same kind of thing can be said of a brain dead person.Until we recognise that perceptions differ amongst people surrounding a brain dead person, we will never understand the essence of the issue of brain death. Are 'persons' limited to those who are 'alive'? I suppose there are many people reading this who feel something is not quite right when they read the words 'brain dead person'.This is because in other books, words like 'the brain dead', 'a brain dead body' and 'a brain dead patient' are used.However these terms do not express clearly the aspect I want to emphasize - the 'person' who is in a state of brain death. [13/14] But using my phrase will probably encourage further objections, namely, the idea that there can be a 'brain dead person' is in itself quite strange.The objection goes that, the moment a person becomes brain dead, they die, and so it is unscientific and mistaken to call the dead body a 'person'.I will discuss shortly whether it is actually unscientific or not, but since the objections are serious I would like to consider them briefly. To people who raise such objections, I would like to respond by asking the opposite question: When people die, what on earth do they become?They will probably answer, 'A dead body'.A dead body is not a person?‘No.’ Then what on earth is it?They will answer: 'A dead body is an object.It is not a person.' I think that this way of thinking is being contested by the issue of brain death.If a dead body is an object, then when we die we become 'objects'.When humans are alive, they are 'people', but when they die they become 'objects'.This implies that 'being alive' and 'being a person' are one and the same.But is this really so? There is such a thing as a 'dead person'.What could this identify? According to the idea that all dead people become objects, the concept of a 'dead person' is a fundamentally impossible logical contradiction. But we can use the phrase 'dead person' in everyday life, and we do not feel any contradiction when we do so.We can say 'a dead person' to mean a dead body.This means that some dead bodies are regarded as 'persons'. [14/15] This is an important point - we regard some dead bodies as 'persons'. In other words, when we consider life and death we have two categories, 'living persons' and 'dead persons'.'Living persons' and 'dead persons' are in totally different conditions, and their relationships to us are also totally different.However the one thing they have in common is that they are both 'persons'. There is anotherway of categorising 'persons'.Previously, I categorised persons into three kinds:
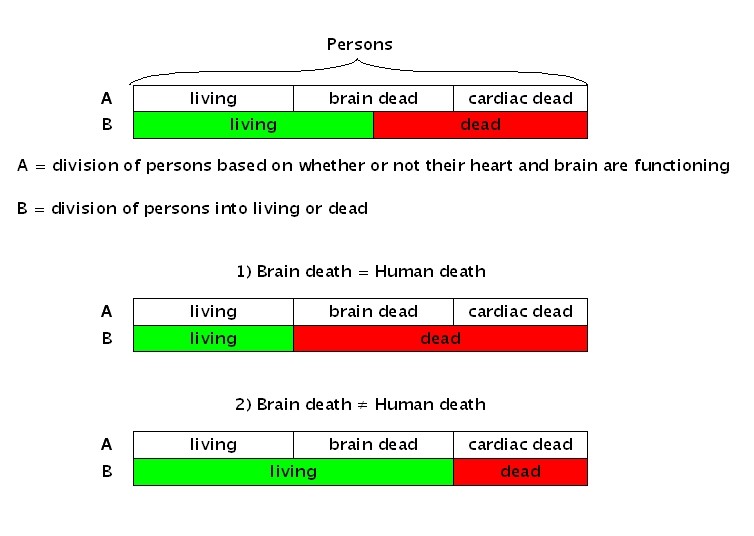
We would say that 1) is a 'living person', even including those who are sick.2) is a 'brain dead person', and 3) is a 'cardiac dead person'.If we concentrate on the functionality of the heart and brain, we can divide people into these three kinds.The nature of each kind differs significantly from the others.However the one point they all share is that they are all regarded as 'persons'. The problem of whether or not brain death is human death is often the subject of debate.This is nothing other than the problem of how to resolve these two ways of categorising 'persons'. Please look at figure 1. |
 |
|
When Ais taken together with B there are two possible outcomes.The view that brain death is human death is represented by 1), while 2) represents the view that brain death is not human death. Whether or not brain death is human death is not considered to be a major ethical problem, apart from legal issues such as inheritance, wills and the desecration of corpses. [15/16]The real ethical problem is not whether or not a brain dead person is dead or alive, but how we should conduct our relationships with brain dead people. (Please see An Invitation to the Study of Life, Keiso Shobo, April, 1988, esp. Chapter 8, “Discourses and Ethics on Brain Death,” which elaborates on brain death, and the life and death of human beings.) Human relationships surrounding a brain dead person Since long ago, we have held ideas about to conduct our relationships with other people.These have become part of our culture and traditions over time.For example, we display minimum standards of conduct towards others with whom we associate in society.'Standards of conduct' might be an exaggeration, but I mean the kind of things we do every day, such as refraining from hurtful language when we talk to others, not suddenly turning up on someone's doorstep uninvited, receiving presents with a smile and so on.This might also include respecting each other's right to life.These kinds of repeated associations with the people around us make up our moral traditions.Of course, these traditions have also changed many times throughout history. The way we relate socially to cardiac dead people can be seen in exactly the same way.You might be surprised at the idea of 'relating socially to cardiac dead people', but take for example, funerals.In our society, when a person dies [16/17] (when they become cardiac dead) we hold an important event known as a funeral.At funerals, relatives and acquaintances are invited to offer incense. The wake is performed, and after the final farewell, the coffin is carried away to be cremated.[This is a typical Japanese funeral. - Trans.]The procedure of a funeral service differs according to area and time period, but in all cases there are social ceremonies where people gather around the cardiac dead person and perform funeral rites which are passed down from generation to generation. Clearly the funeral serves to unite the bereaved relatives and the local community.However a funeral is not just simply a social event.It is a mutual support network, created so that the cardiac dead person's soul may reach the next world unharmed, and also to allow the family to accept the death of their relative (actually, priests and monks also have a certain interest in funerals).A funeral consists of the person to person relationships centered around a cardiac dead person. [17/18] And as far as there are person to person relationships, there are also minimum standards of conduct and behaviour.For example, treating the dead person's body with respect, not speaking ill of the dead, trying not to disturb the bereaved family emotionally, and refraining from behaviour that would disrupt the sombre atmosphere of the funeral.These minimum standards of conduct have been passed down through the ages, and allow the family to accept the death of their kin with relative ease, and thus we may come to believe that the soul has been sent unharmed into the next world. So whether towards the living or the dead, person to person relationships in our society have minimum standards of acceptable conduct which are created and passed down through the generations.Now, someone who is brain dead is also a person.Therefore we should create and pass down shared minimum standards of acceptable conduct with regards to how families, doctors, nurses and people related to transplant operations should behave when they come into contact with brain dead persons, no matter how long this may take.This is what the issue of brain death is really about. Shohei Yonemoto has stated the following, not only with reference to brain death, but also the broader issue of bioethics.
Yonemoto argues that ethical discussion in Japan should deepen discussion about forms of culture and rules for dealing with new technologies. This perspective is similar to that of Tatsuo Inoue, who reformulated 'justice' as 'rules' of cohabitation. (Rules of Cohabitation, Sobunsha, Jun., 1986).I sympathize with these ideas. [18/19] I believe that part of the current social confusion surrounding brain dead death and organ transplantation is due to the fact that these forms and rules, as referred to by Yonemoto, have not been established in a way that is acceptable to all of society.In other words, we do not have minimum shared standards of acceptable conduct regarding how we behave with respect to brain dead people, and this causes all kinds of ethical problems. The most important point is that brain dead people are persons, and that brain death consists of person to person relationships. In other words, the ethical problem of brain death is the question of how to establish a kind of 'cohabitation' between ourselves and brain dead people.By creating a society in which we can cohabit with 'brain dead persons' we would also be creating one where we could cohabit with, for example, 'disabled persons' and 'persons with senile dementia'. It now becomes clear that before discussing organ transplants, another ethical issue arises and needs to be dealt with - the question of how we should conduct our social relationships within the ICU, where brain dead people spend most of their time.That is to say, ethical issues in the ICU.
(End of Chapter 1) >> Go to Chapter 2 Commentary on this chapter/book >> Commentary on "Brain Dead Person" Chapter 1 by Robert D. Truog, MD [Nov.24,2001] *For more information, visit Brain Death and Organ Transplantation in Japan. |